Infectious Diseases Case of the Month #23 |
|||
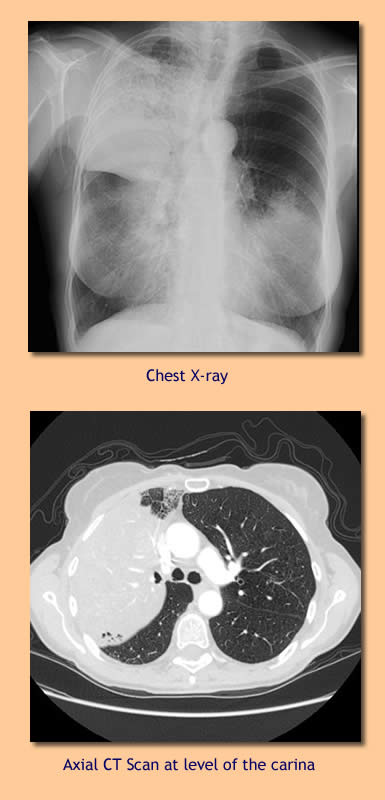 |
A 65 year old white female retired RN was admitted to the hospital for chronic pulmonary infiltrates, cough, and hypoxemia. Previously healthy, a former smoker (she quit in 1980), she had first become aware of an annoying cough twenty months prior to admission. Initially she believed that it represented a cough related to "post-nasal drip." Eight months prior to admission she and her husband embarked on a four month long round the world trip which would involve visits to China, Thailand, Cambodia, Australia, Easter Island, Egypt and Europe. At about the time of her return from this trip her cough became notably worse and productive, and she first sought medical attention. During an evaluation at a local hospital her CXR showed an large area of consolidation involving her right upper lobe. CT scan showed a dense consolidation likewise in the RUL with smaller infiltrates in the RML and RLL as well as in the lingula of the left upper lobe. She was treated with antibiotics including levofloxacin, ceftriaxone, and azithromycin. Sputum smears and cultures and legionella and pneumococcal urinary antigens were non-diagnostic at the time of her initial evaluation. However, several weeks later an AFB culture obtained at the time of her initial evaluation was reported positive. She was begun on isoniazid (INH), rifampin, and ethambutol. Subsequently, the acid fast organism was identified as Mycobacterium gordonae. Azithromycin was substituted for INH, and rifampin and ethambutol continued. Additional sputa for AFB were ordered to see if Mycobacterium gordonae might be consistently recovered. Despite therapy she continued to have a productive cough and continued to experience weight loss (20 pounds cumulatively over the preceding several months). She may have had low grade fevers but did not experience chills or sweats. She became progressively more hypoxemic, and as a consequence, was admitted to the hospital for further evaluation. On admission she was afebrile and did not appear to be in distress. Lungs were clear to auscultation. Laboratory evaluation included WBC 6.4, Hgb 14.7. Arterial blood gas (room air) revealed pH 7.45, pCO2 33, pO2 67. CXR and CT scan are pictured at left. In addition to the RUL disease pictured there there also continued to be lesser consolidative changes in the RML, RLL, and lingula of the LUL. Extent of disease appeared to have progressed since prior CT scans. The radiologist favored an inflammatory etiology as there was no volume loss, evident airway compromise, or evident hilar or mediastinal adenopathy. The patient underwent bronchoscopy with with BAL and transbronchial biopsies. The examining pulmonologist noted thin, non-purulent secretions and essentially normal, patent airways. |
||
What was the likely cause of this patient's illness? |
|||
 |
Transbronchial biopsy specimens were consistent with adenocarcinoma with bronchioloalveolar features. Pictured at left are high power photomicrographs of the patient’s transbronchial biopsy showing normal respiratory epithelium (L) and adenocarcinoma with bronchioloalveolar features (R). In contrast to the normal ciliated pseudo-stratified respiratory epithelium, the abnormal tissue shows atypical, haphazardly arranged cells with prominent nucleoli without cilia. Although not appreciated in the photo of the adenocarcinoma (R), the normal architecture of the respiratory epithelium was preserved and, thus, the descriptor, “with bronchioloalveolar features.” Mycobacterium gordonae failed to again grow on subsequent sputum cultures (after the original positive culture). This organism is generally considered nonpathogenic and is the most frequently isolated mycobacterial contaminant. It is readily isolated from freshwater, pipelines, and laboratory faucets. Mycobacterium gordonae has rarely been a cause of disease. When disease has been described, it has primarily occurred in persons with underlying immunosuppression such as in persons with AIDS, persons on chronic corticosteroids, or in cases of malignancy. In the case described the patient did not respond to therapy likely to have been effective for M. gordonae, and biopsies did not suggest an infectious etiology for her infiltrates. The other choices listed in the original vignette could have been the cause of chronic pneumonia. In general, all these infections might have been expected to have more prominent constitutional symptoms (fever, chills, sweats, etc) than this patient experienced. Burkholderia pseudomallei is an aerobic gram negative bacillus, the causative agent of melioidosis, classically endemic in regions including Southeast Asia, China, portions of Australia, and the Indian subcontinent. Illness ranges from acute fulminant pneumonic/septicemic infection to subacute/chronic infection involving multiple organs. Blastomyces dermatitidis can be a cause of subacute to chronic mass like pulmonary infection and is endemic in northern Michigan (see Case of the Month #15). Mycobacterium tuberculosis can clearly cause chronic pulmonary disease, but as already mentioned, would have been expected to have more prominent associated constitutional symptoms. Ref: Griffith, DE, et al., An official ATS/IDSA statement: diagnosis, treatment, and prevention of nontuberculous mycobacterial diseases, Am J Crit Care Med, Vol 175. pp 367-416, 2007 |
||
| Home Case of the Month ID Case Archive | Your Comments/Feedback | ||